Gut Microbiome Therapy Targets Serotonin for Depression Relief
Your gut and your brain are in constant conversation. Most people don’t realize that roughly 90% of the body’s serotonin is produced in the gastrointestinal tract - not the brain. That fact alone has pushed researchers and clinicians to rethink how depression gets treated. Gut microbiome therapy is emerging as a serious contender in mental health care, and the approaches vary widely in evidence, accessibility, and cost.
This is a look at some of the most promising gut microbiome interventions being studied or used for depression, with honest notes about where the science stands for each one.
Targeted Probiotic Strains (Psychobiotics)
Psychobiotics are specific bacterial strains selected for their ability to influence mood through the gut brain axis. The most studied strains include Lactobacillus rhamnosus (JB-1), Bifidobacterium longum 1714, and Lactobacillus helveticus R0052 paired with Bifidobacterium longum R0175.
A 2019 randomized controlled trial published in Translational Psychiatry found that participants taking B. longum 1714 for four weeks showed reduced cortisol output and lower self-reported stress compared to placebo. The effect sizes were modest but consistent across multiple measurements. A separate Iranian trial in 2020 showed that patients with major depressive disorder who took a multi-strain psychobiotic alongside their SSRI had 45% greater improvement on the Hamilton Depression Rating Scale than those on SSRI plus placebo.
The appeal is clear: probiotics carry minimal side effects and don’t require a prescription. But strain specificity matters enormously. A generic probiotic from a drugstore shelf won’t replicate what these trials used. Clinicians who recommend psychobiotics should be able to name the exact strain and dosage backed by clinical data.
Skip if… you’re looking for rapid symptom relief. Psychobiotic effects take weeks to emerge, and they’re best understood as adjunctive - meaning they work alongside existing treatment, not as a replacement.
Fecal Microbiota Transplantation (FMT)
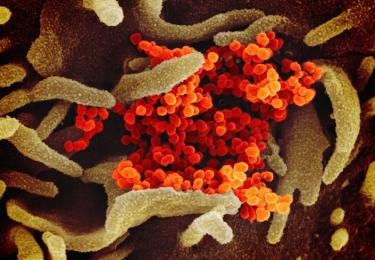
FMT involves transferring stool from a healthy donor into the gastrointestinal tract of a recipient. It sounds extreme. It is, honestly, still somewhat experimental for psychiatric conditions. But the rationale is grounded in solid biology.
Animal studies have been striking. In a well-known 2016 experiment, germ-free mice colonized with gut bacteria from patients with major depression developed depressive-like behavior - reduced sucrose preference, increased immobility in forced swim tests. The reverse also worked: microbiota from healthy donors reduced depressive behavior in previously colonized mice.
Human data is thinner. A small Australian pilot study from 2023 treated 15 patients with treatment-resistant depression using FMT capsules and reported significant improvement in 8 of 15 participants over 12 weeks. Promising, but uncontrolled and tiny. Several larger randomized trials are underway.
FMT is currently FDA-approved only for recurrent Clostridioides difficile infection. Using it for depression remains off-label and largely inaccessible outside research settings.
Skip if… you want something available right now through your regular doctor. FMT for depression is still a research-stage intervention with limited clinical access.
Dietary Microbiome Modification
The simplest and most accessible microbiome intervention isn’t a supplement or procedure. It’s food.
The SMILES trial, published in BMC Medicine in 2017, remains one of the strongest pieces of evidence here. Participants with moderate to severe depression who followed a modified Mediterranean diet for 12 weeks showed significantly greater improvement than those receiving social support alone. About 32% of the diet group achieved remission, compared to 8% of controls. The dietary protocol emphasized whole grains, legumes, fermented foods, vegetables, fruits, nuts, and olive oil - all known to promote microbial diversity.
Fermented foods deserve specific mention. A 2021 Stanford study found that a 10-week high-fermented-food diet increased gut microbiome diversity and decreased 19 inflammatory markers. Foods like kimchi, yogurt, kefir, sauerkraut, and kombucha drove those results.
Prebiotic Fiber Supplementation
Prebiotics feed the bacteria already living in the gut. Galactooligosaccharides (GOS) have shown the most psychiatric relevance. A 2015 Oxford study found that GOS supplementation reduced waking cortisol levels and shifted attention away from negative stimuli - patterns that mirror the effects of some anti-anxiety medications.
The connection to serotonin is direct. Short-chain fatty acids produced by bacterial fermentation of prebiotic fiber stimulate enterochromaffin cells to produce serotonin. More diverse fiber means more diverse microbial metabolism means greater serotonin precursor availability.
GOS supplements are commercially available and inexpensive. So are high-prebiotic foods: garlic, onions, leeks, asparagus, bananas, and oats.
Vagus Nerve Stimulation via Microbiome Pathways
The vagus nerve is the primary physical highway between gut and brain. About 80% of its fibers carry information upward - from gut to brain, not the other way around. Certain gut bacteria produce metabolites that activate vagal afferent neurons, which then signal brain regions involved in mood regulation.
Research groups are exploring whether microbiome-targeted interventions can achieve effects similar to direct vagus nerve stimulation (VNS), which is already FDA-approved for treatment-resistant depression. The idea: instead of surgically implanting a device on the vagus nerve, shift the microbial composition to naturally increase vagal tone.
This remains theoretical for now. No clinical trials have directly tested microbiome modification as a VNS alternative. But the mechanistic pathway is well-established in preclinical work.
Microbiome Testing and Personalized Protocols
Companies like Viome, Ombre, and Thorne offer direct-to-consumer gut microbiome testing. They sequence microbial DNA from a stool sample and generate personalized supplement and dietary recommendations.
The technology is real. The clinical utility for depression is unproven. No peer-reviewed study has demonstrated that following a personalized microbiome report leads to measurable improvement in depressive symptoms. The tests also suffer from significant variability - the same sample sent to two different companies can yield meaningfully different results.
That said, the data can be interesting as a baseline. Some functional medicine practitioners use microbiome testing alongside standard psychiatric assessment to identify extreme dysbiosis or pathogenic overgrowth that might contribute to inflammation-driven mood symptoms.
Synbiotic Formulations
Synbiotics combine probiotics and prebiotics in a single supplement, aiming to both introduce beneficial bacteria and feed them simultaneously. A few formulations have been developed specifically for mood support.
A 2022 systematic review in Nutrients examined seven RCTs and found that synbiotic supplementation was associated with small but statistically significant reductions in depression scores. The quality of evidence was rated moderate. Most trials lasted 8-12 weeks and used varying formulations, making it hard to identify which combinations work best.
Synbiotics are commercially available and carry a safety profile similar to standard probiotics. They’re a reasonable addition for someone already pursuing dietary and probiotic approaches who wants a combined product.